New Cost Cap industry-driven committee gets going
Members of the Office of Health Strategy’s (OHS) latest committee to drive down the growth in Connecticut’s healthcare spending moved past their initial reluctance to engage in their November and December meetings. OHS expects the provider and insurer-dominated committee to agree on ways to reduce their own costs/profits. Hopefully, they do not also use the committee as a forum to disadvantage competitors.
Unlike other states’ Cost Cap committees, Connecticut’s has no consumer advocate members. Connecticut’s committee is much heavier on provider/health system and state agency members than other states.
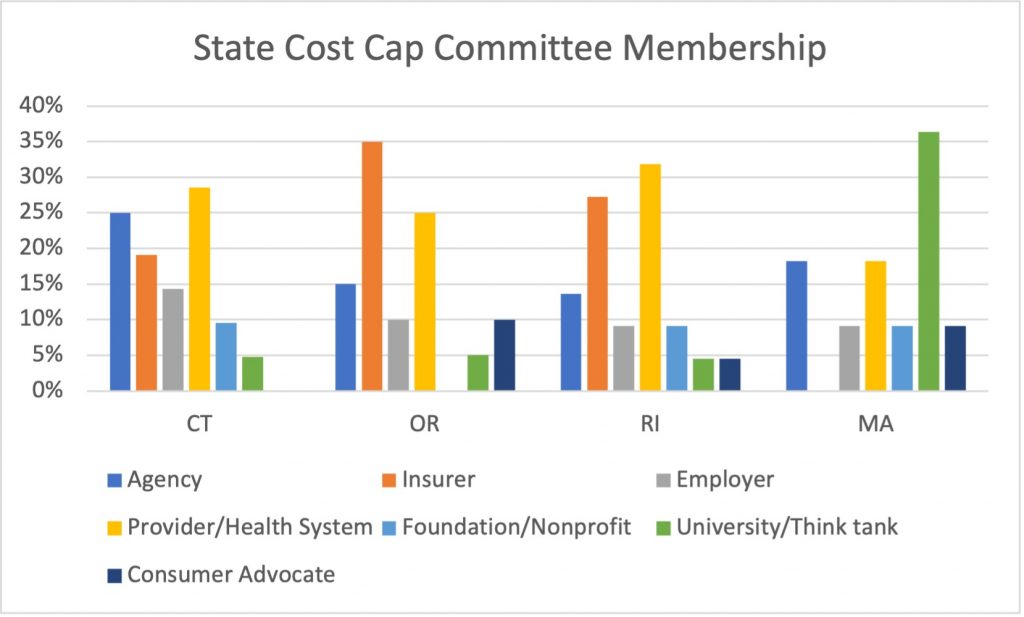
Sources: Connecticut, Oregon, Rhode Island, Massachusetts
The November meeting opened with OHS’s consultants saying, “We want you to feel ownership of this process.”
Medicaid “under payment” was blamed by all the industries at the table for driving up other payers’ prices, despite evidence to the contrary. Committee members also pushed for alternative payment models, shifting financial risk onto providers. Regarding OHS’s controversial Primary Care Roadmap, the members were generally supportive. However good questions included how primary care providers are expected to lower costs for critically ill patients that are often in the hospital, who should have to pay the increased investment in primary care and what portion will providers or insurers pay, what reductions in costs can payers expect for the increased spending, why would insurers make long-term investments they may not benefit from as patients move programs and payers, how to ensure they aren’t paying more for things they already pay for, and how will OHS measure that the goals are being met, that the investments are working. Members noted that the Roadmap envisions a large increase in responsibilities for stressed primary care practices. Reportedly, employers are not sure why they should pay more on top of already high costs for health care.

