Medicaid switch from MCOs saving taxpayers billions

If Medicaid per member per month costs had held steady at 2012 levels, taxpayers would have spent $2.25 billion more by last year.
As with most health care in Connecticut, Medicaid spending was rising quickly before 2012 growing by almost half over the prior four years. But in 2012, Connecticut made a remarkable and unique move — Medicaid switched from a capitated payment model using private insurers to a care coordination-focused, self-insured payment model. Since then, state spending on Medicaid has decreased, saving $400 million last fiscal year and leading the nation in cost control. The shift also resulted in significant improvements in quality, access to care, provider participation and consumer satisfaction. At the same time enrollment in the program has grown by 300,000 members. Connecticut Medicaid accomplished this with a remarkable $6 million decrease in administrative funding.
Unfortunately, that progress remains politically fragile, requiring continued commitment by state policymakers to our successful model and resisting a return to private insurers.
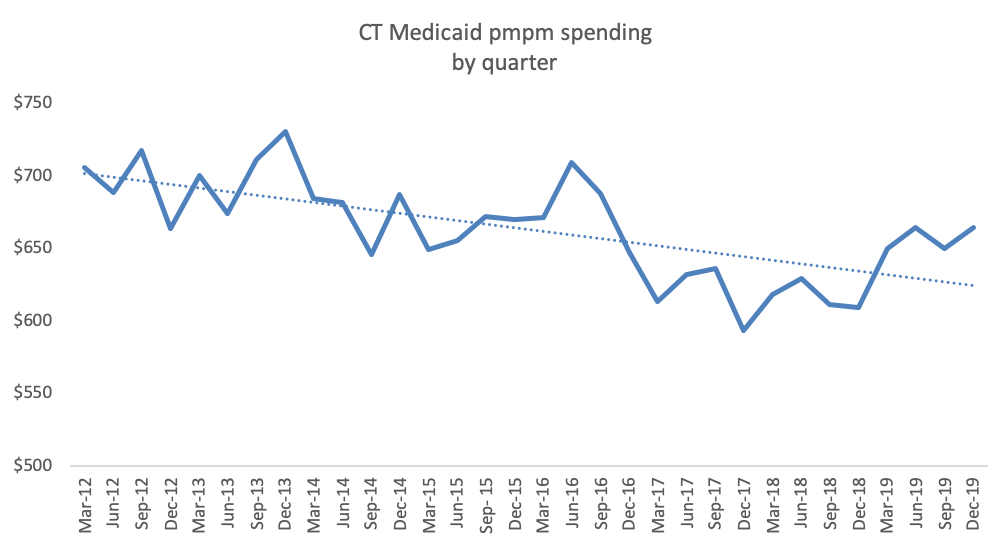
Connecticut Medicaid per member per month costs (pmpm) are down 6%, from $706 in the first quarter of 2012 to $664 in the last quarter of 2019. Connecticut Medicaid’s per enrollee costs were ninth highest among states in 2011 but down to 17th by 2018.
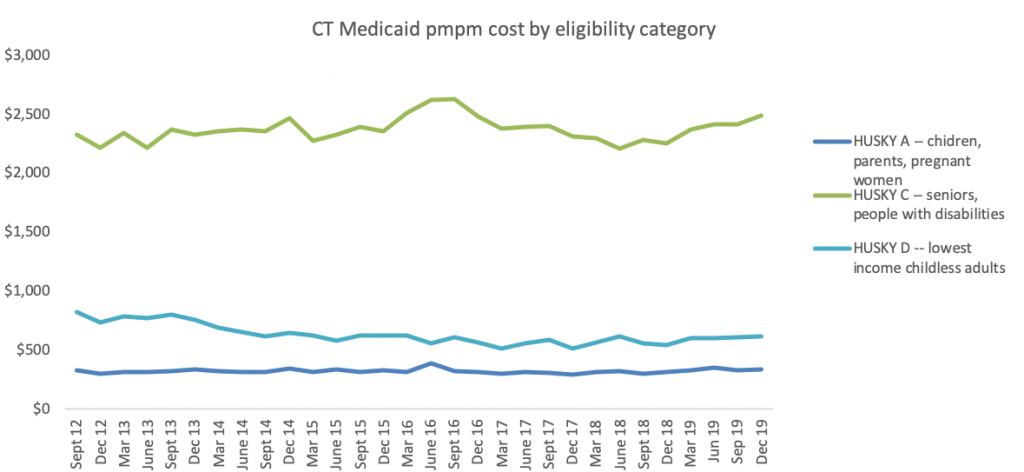
Connecticut Medicaid per member costs have been stable or declining across eligibility categories, including newly eligible childless adults, children/families, and seniors/people with high medical bills. Lower total per member costs are not the result of an influx of healthier new members.
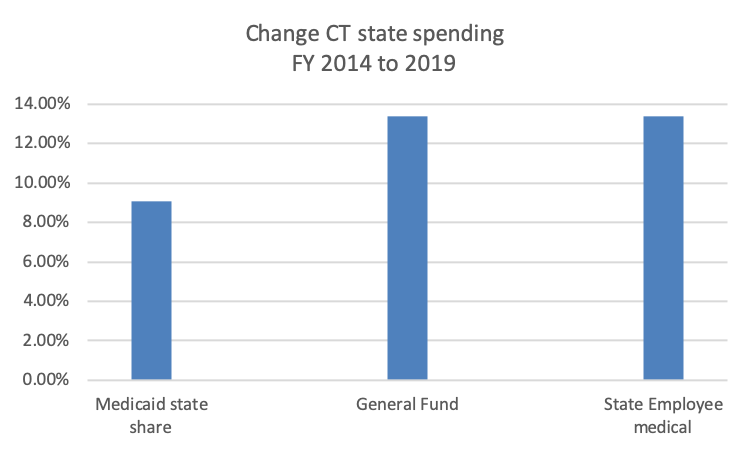
Medicaid is not the driver of Connecticut’s growing state budget. Connecticut’s total state share of Medicaid costs has risen less quickly than the total General Fund or health care costs for state employees and retirees.
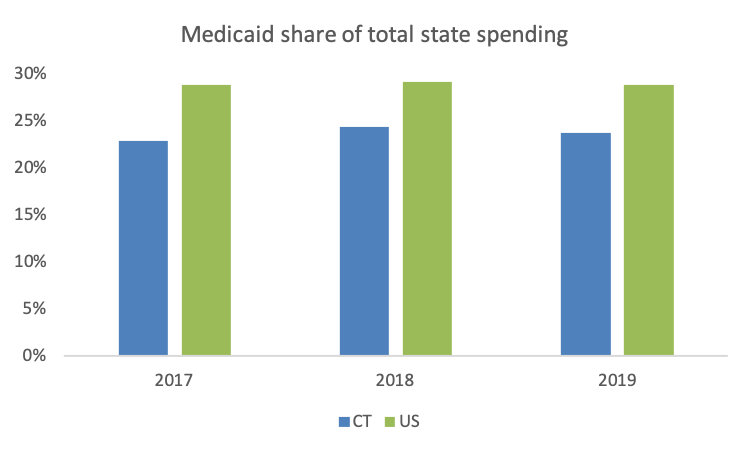
Connecticut spends less of our state budget on Medicaid than other states, spending 23.8% on Medicaid in 2019, well below other states averaging 28.9%.
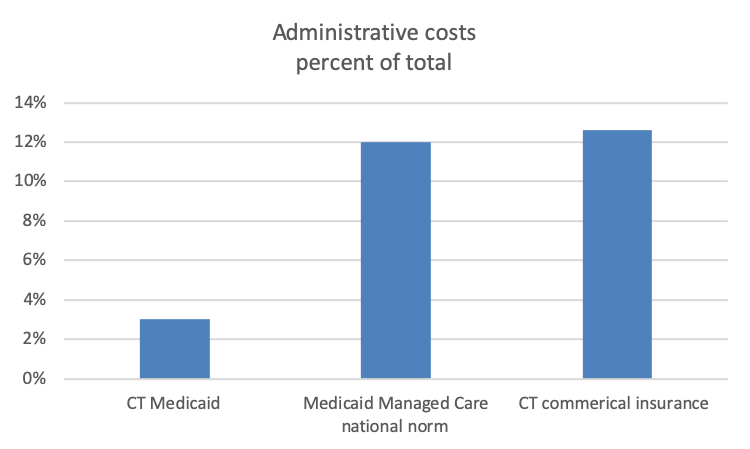
Connecticut Medicaid spends only 3% of total costs on administrative expenses. In contrast, Medicaid managed care plans in other states and Connecticut commercial insurance plans average 12% or more to administrative costs and profits.
Bottom Line: Medicaid is not driving either rising health costs in Connecticut or the state’s budget growth. In fact, Medicaid has provided significant relief to both state and federal budgets since leaving the managed care model.
Sources:
DSS financial presentations to MAPOC – February 2020, February 2019, February 2018, January 2016, October 2015, October 2014
Annual Reports – Budgetary Basis, Office of State Comptroller
State Expenditure Report FY 2017 to 2019, NASBO
2018 Consumer Report Card on Health Insurance Carriers in Connecticut, CID

