Connecticut Medicaid costs stable but rising physician and clinic spending threaten progress
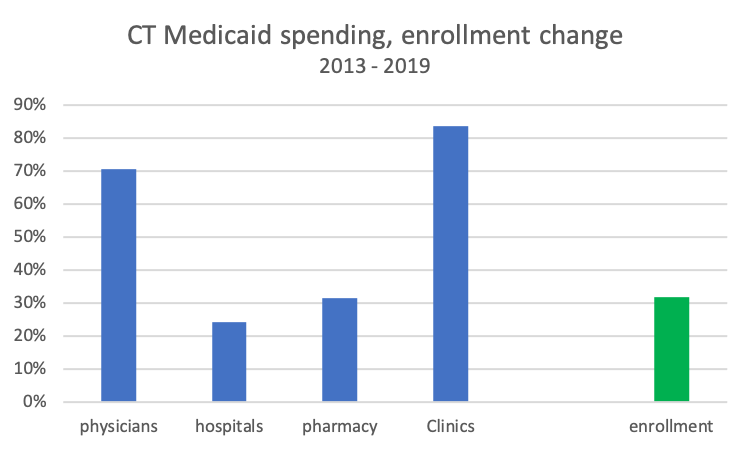
Since switching from managed care organizations in 2012 to focus on care management, Connecticut Medicaid spending has stabilized while enrollment has expanded significantly, according to the state’s latest financial report. Medicaid now covers one in four state residents. However, physician and clinic spending increases are eroding early progress in controlling costs.
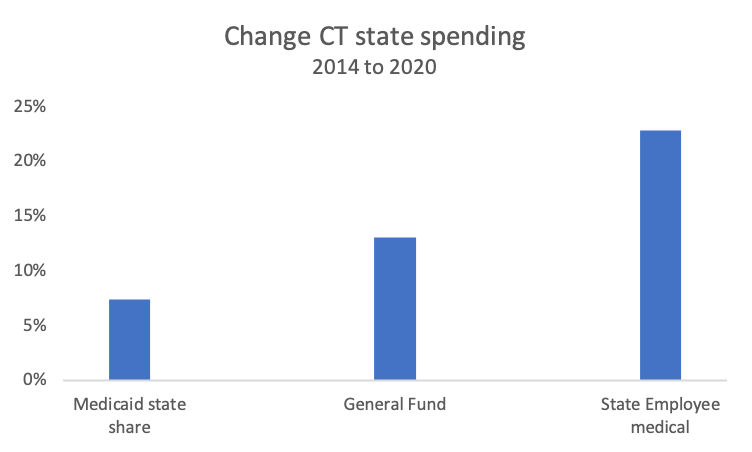
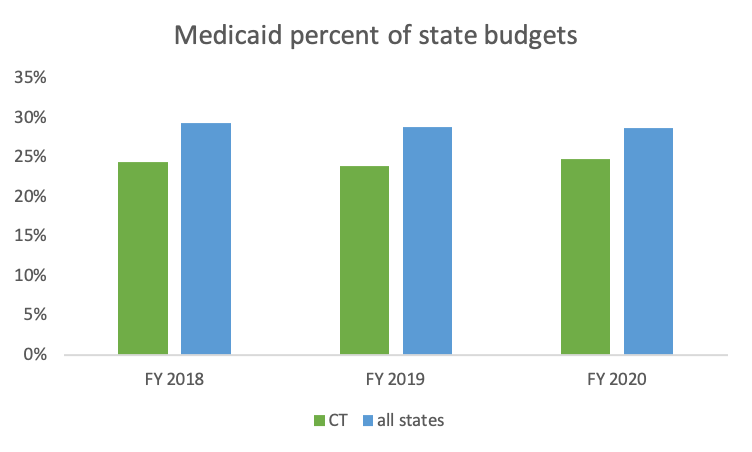
Medicaid is not the source of rising costs to taxpayers. State spending on Medicaid has lagged significantly behind increases for state employee health benefits and total General Fund spending. Connecticut spends less of our state budget on Medicaid than most states. Since 2014, federal Medicaid matching funding to Connecticut has increased significantly.
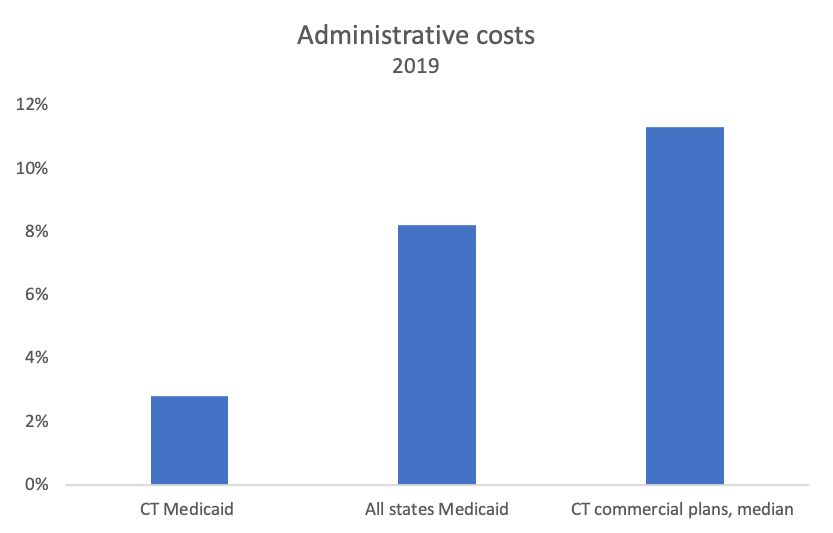
Connecticut Medicaid is very efficient. Administrative burden in the program is 3-fold lower than for other state Medicaid programs and 4-fold lower than Connecticut commercial insurance plans. This is likely because, unlike other states, Connecticut Medicaid no longer uses private, for-profit insurers to run our program.
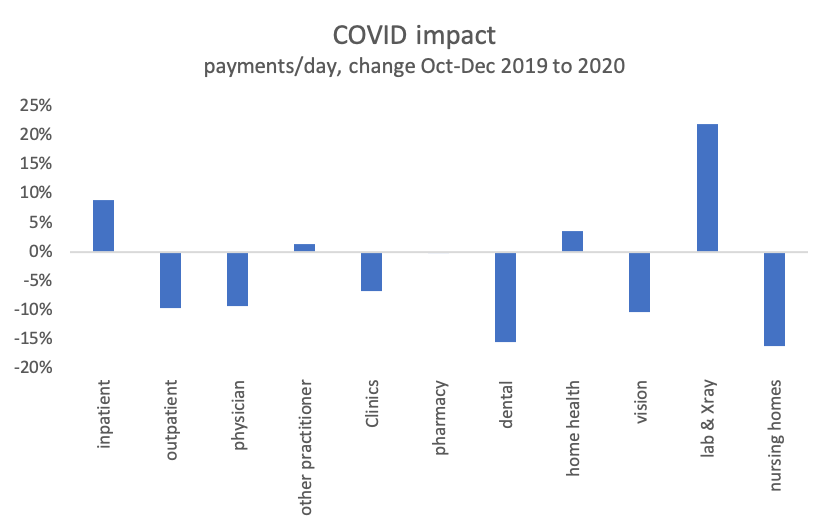
As for the rest of our state’s health system, the COVID pandemic has impacted Connecticut Medicaid. However, by the end of 2020 most sectors were back up to, or exceeded, pre-pandemic levels.
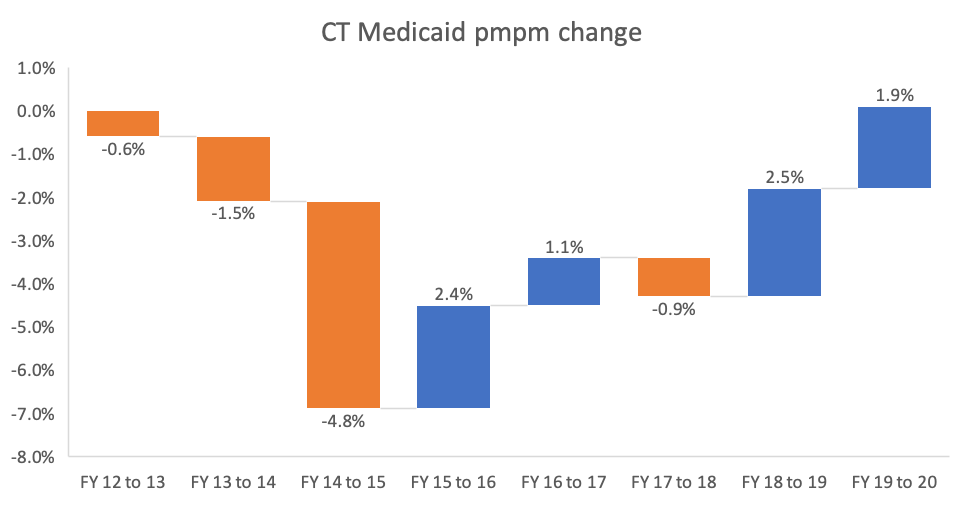
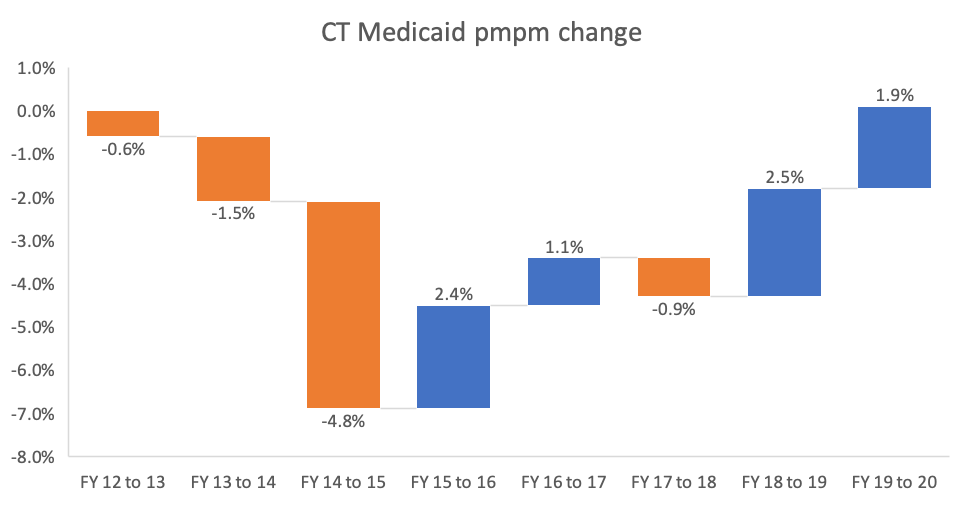
Per member spending in Connecticut’s Medicaid program dropped significantly in 2013, 2014 and 2015, after switching from managed care. However, per member spending has slowly increased since 2015. However, at $8,890 Connecticut Medicaid per member costs have kept in step with other states. According to the federal Centers for Medicare and Medicaid Services, in 2018 Connecticut ranked 19th highest in per member costs, down from 18th the year before.
Between 2013 and 2019, Connecticut Medicaid enrollment grew 32% but physician spending grew 71% and clinic costs were up 84%. Pharmacy costs kept pace with enrollment growth while hospital spending lagged slightly.
Medicaid is not the driver of rising state spending. Connecticut Medicaid costs have grown less quickly than state employee/retiree health benefit spending or the total General Fund.
The federal share of Connecticut Medicaid spending rose to 60% last year, up from 55% in 2014. Variations were due to the stepped reduction in the expansion population match rate under the Affordable Care Act and the COVID match increase in 2020.

Our state spends less of our state budget on Medicaid than other states. Last year, 25% of Connecticut’s General Fund went to Medicaid compared to 29% average for all states.
At 2.8%, Connecticut Medicaid’s administrative burden is well below other state Medicaid programs averaging 8.2%, or Connecticut commercial insurers with 11.3% median administrative costs.
COVID has had a substantial impact on Medicaid and the rest of Connecticut’s health system. However, by the end of 2020, Medicaid spending was returning to pre-pandemic levels across sectors. Four sectors have exceeded pre-pandemic spending. Dental and nursing home spending levels are lagging, likely for different reasons.