Connecticut hospital systems vary in reducing low-value care
A new report published in JAMA Internal Medicine on low-value care provided to Medicare beneficiaries at the health system level offers actionable tools to improve effective care on the ground. Healthcare services that provide little or no health benefit, may harm patients, increase costs, and waste resources are low-value. Examples include prostate specific antigen testing in men over 70 years old, unnecessary pre-surgery tests and imaging, and use of anti-psychotic medications for patients with dementia. Despite decades of effort, over one fifth of all healthcare provided in the US is low-value, wasting hundreds of billions of dollars every year for patients and society. Reducing low-value care offers one of the best options to responsibly lower healthcare costs while improving health outcomes.
The new study measured the use of widely recognized 41 low value services across 556 US health systems serving 11.6 million Medicare beneficiaries, including nine health systems in Connecticut. The authors found that lab tests and drugs account for most low-value care. Low-value care is more likely in systems without teaching hospitals, with fewer primary care physicians, high healthcare spending communities, for-profit health systems, those with more Medicare members who are also eligible for Medicaid, and those that serve more non-White patients. Northeastern health systems generally performed better than the US average. Unfortunately, ACO status had no influence on low-value care.
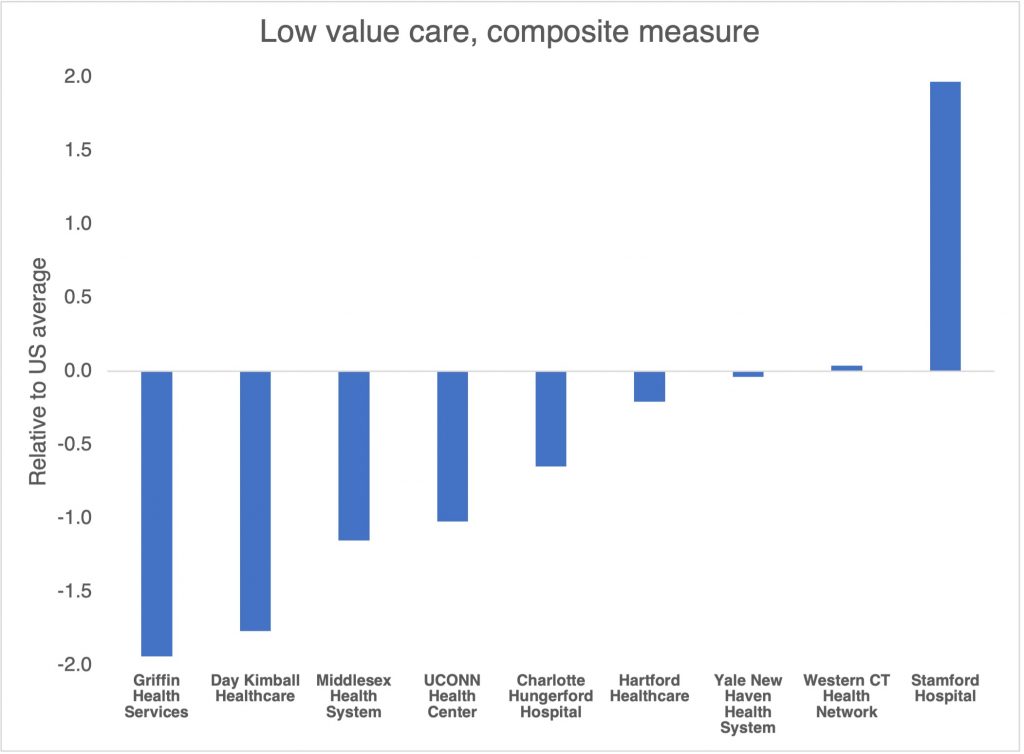
Griffin Health Services led Connecticut in reducing low value care. Stamford Hospital was far worse than other state or US hospitals in low value care. Six Connecticut hospital systems performed better than the US average – Griffin, Day Kimball, Middlesex, UConn, Charlotte Hungerford, and Hartford Healthcare, in that order. Two hospital systems were very close to the US average – Yale-New Haven and Western CT Health Network.
The authors suggest that policymakers and payers can use the information to track progress by health systems to reduce low-value care over time, and systems can use the information to inform improvement. For example, as lab tests are a large share of low-value services, health systems could use the information to revise standard order sets. State and regional health improvement leaders could use the measures in educating providers. Health systems could use the measures to design provider incentives to reduce unnecessary care, educate providers, and use in hiring and retention decisions. Health plans could include the measures in contract targets and to create networks of high-value clinicians. Public reporting could help patients understand where they are likely to get higher value care.

