Community health center quality behind the rest of Medicaid

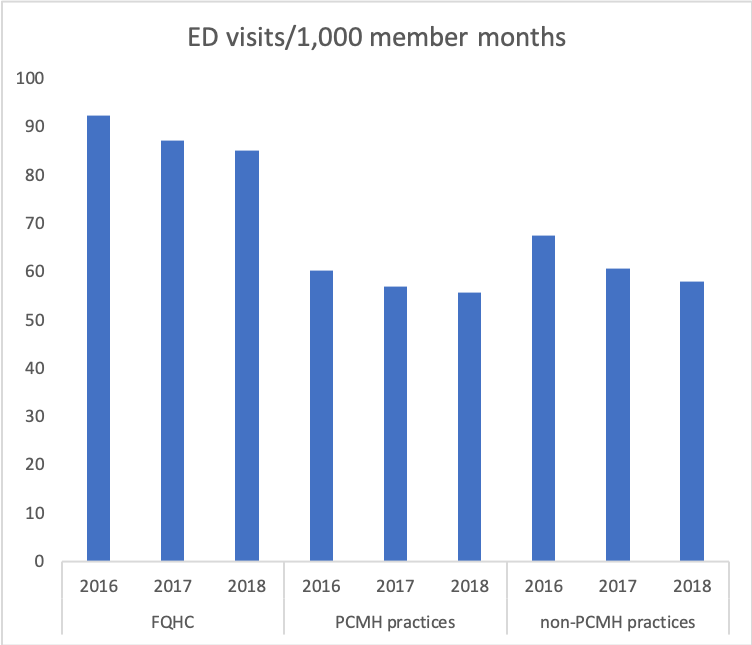
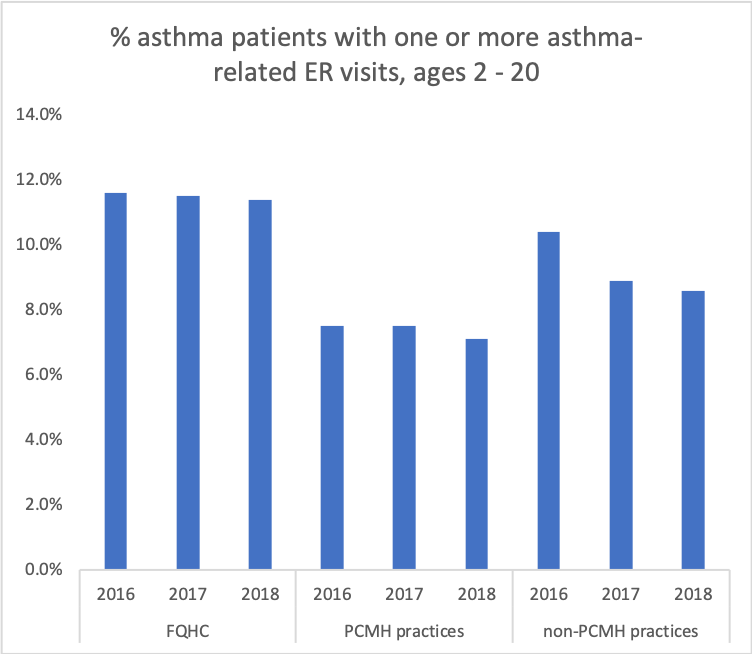
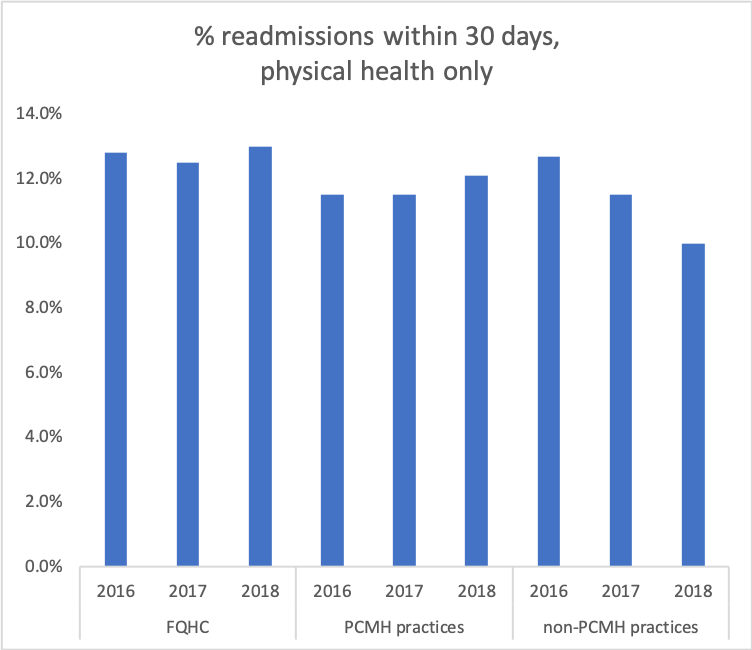
The good news is that Medicaid health outcome quality measures generally improved in all practice setting from 2016 through 2018. Unfortunately, community health centers (FQHCs) are not doing as well as their counterparts, either other Patient-Centered Medical Home practices (PCMHs), or non-PCMH practices in serving Medicaid members. This data comes from CHNCT’s report to MAPOC in December and subsequent updated data from DSS, but it reflects lower FQHC performance in 2015 as well. We compared the three Medicaid health metrics that measure outcomes among the 12 measures reported – ED visits, ED visits by members with asthma, and hospital readmissions within 30 days of discharge. For all three measures, lower rates are better.
In all three years, Medicaid FQHC patients were more likely to visit an ER than Medicaid patients cared for by either PCMH or non-PCMH practices. While all practices are slowly lowering patient ED visits, at the current rate of improvement, it would take over 150 years for FQHC performance to catch up to PCMHs and they will never catch up with non-PCMH practices.
In all three years, FQHC Medicaid members with asthma were more likely to visit the ER than other Medicaid members. While these rates are also dropping, FQHCs are making progress more slowly than either PCMHs or non-PCMH practices.
Contrary to ED visits, Medicaid hospital readmission rates are more similar between FQHCs and other practices. However, Medicaid FQHC patients are more likely to be readmitted to a hospital than either Medicaid PCMH or non-PCMH practices, and the rate is getting worse. Readmission rates for non-PCMH practice patients are the only improvement.
Bottom Line: Community health centers need to improve the quality of care for their Medicaid members.

