Medicaid
COVID hit Medicaid hard
Medicaid members were about 33% more likely to be diagnosed with COVID than other Connecticut residents, according to CHNCT’s presentation Friday to the Medicaid oversight council. The average age of members with COVID was 52 years but ranged from newborn to 102 years old. Like the rest of the population, COVID hit Medicaid members with…
Read MoreCost cap committee excludes patients’ provider choices from primary care spending increase
On Thursday, the main committee convened by the Office of Health Strategy (OHS) met to continue their work to set a cap on how much healthcare costs can increase and, at the same time, double spending on primary care. At the meeting they codified a narrow definition of primary care provider for purposes of calculating…
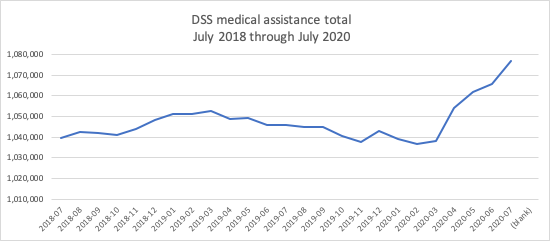
Read MoreMedicaid rolls up 3.9% since February
The number of people getting medical assistance through the state is up by 40,158 or 3.9% from February to last month, according to new numbers from DSS. This was expected as people lose jobs and the employer-sponsored coverage that comes with those jobs. With less income more state residents were expected to qualify for Medicaid.…
Read MoreCost Cap committee considers who qualifies for increased primary care spending
In response to stakeholder feedback that the prior Cost Cap levels were unrealistic and risk unintended harm to patients, at their last meeting the Office of Health Strategy’s Cost Cap committee slightly softened the cap levels. The committee continued their discussion of which providers qualify as primary care providers. OHS wants to significantly increase the…
Read MoreComprehensive updated resource on Connecticut’s health landscape from DPH, get involved
Almost one in six Connecticut children are food insecure and the number of state residents newly diagnosed with HIV has been dropping since 2010, according to the Dept. of Public Health’s new 2019 State Health Assessment. In 2017, 14.4% of Connecticut high school students used e-cigarettes, up from 2.4% in 2009. Over one in four…
Read MoreCost cap update – possible easing on growth cap but primary care target proves difficult
In response to concerns from many sources about potential harm to people, the Office of Health Strategy (OHS) is considering easing the proposed caps on the growth of all healthcare spending. In the latest Technical Team meeting, OHS and Bailit, the consultants running the project, said they would consider starting the cap next year higher…
Read MoreHalf of current COVID hospital admissions are Medicaid members
Connecticut Medicaid has taken a serious hit from COVID. At Friday’s Medical Assistance Program Oversight Council meeting, we learned that while hospitalizations went up, outpatient and physician care went down. In May outpatient care spending was down 51% from last year and physician care was down 36%. Those numbers have risen somewhat but are still…
Read MoreCost cap project sets limits on healthcare spending without public input, ignoring pandemic impact
In meetings of the committee setting limits on healthcare spending for all Connecticut residents, it appears the advocates’ sign on letter and detailed concerns about the Office of Health Strategy’s (OHS’s) Cost Cap project were not heard. The plan is being developed by a Technical Advisory Team, with members chosen only by OHS, including some…
Read MoreOHS committee chooses unrealistic cap for CT healthcare costs
The Office of Health Strategy’s (OHS) Technical Team choosing the cap for future Connecticut healthcare costs has decided on a 3.1% allowed increase for next year, dropping over time to 2.7% by 2025. To illustrate the impact of the cost cap, consider the significant variability in Connecticut’s per capita all-payer total healthcare cost increases from…
Read MoreSurprisingly, Medicaid applications are down sharply with the pandemic
At Friday’s MAPOC meeting, DSS reported that HUSKY applications were down 40% in May from a year before. This was unexpected given massive increases in unemployment and predictions of over 100,000 new Connecticut Medicaid members because of the pandemic. In January, February and March, applications ran 15% to 20% higher than last year. But a…
Read More