CT Medicaid compared to other states – What the evidence says
Governor Lamont is reportedly considering a plan to have private insurance managed care plans (MCOs) run Connecticut’s Medicaid program. From 1996 through 2011, Connecticut Medicaid was run by MCOs, and it was deeply troubled. The program ended under pressure from advocates, providers, and legislators. Since the MCOs left Connecticut Medicaid, access and quality of care have improved, and the state has saved billions of taxpayer dollars.
Findings: How Connecticut Medicaid compares with other states now
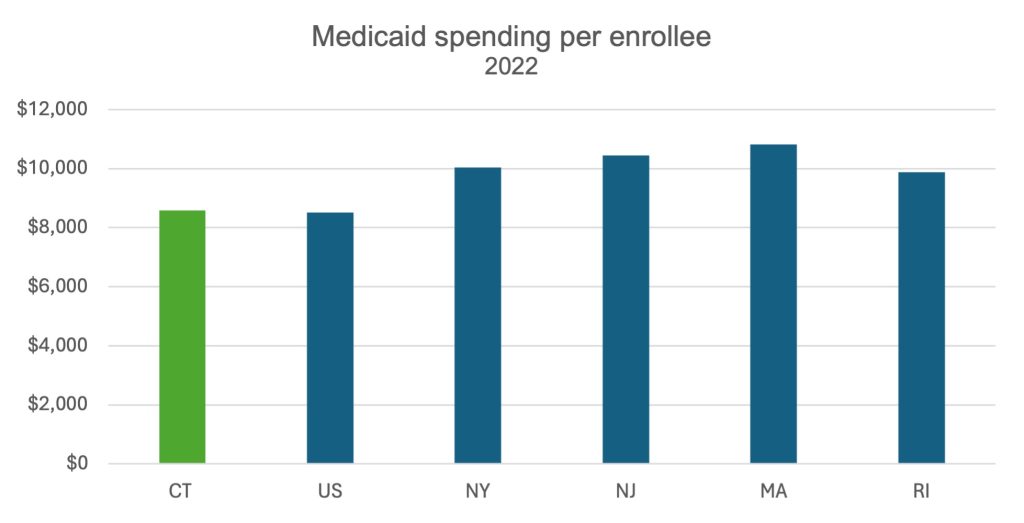
Since removing MCOs, Connecticut’s Medicaid program leads the nation, including comparable states, in cost control and is among the best performing states on quality and access to care.
Connecticut spends far less of our state budget on Medicaid than other states, freeing up $4 billion for other priorities. Connecticut taxpayers benefit by paying one third the administrative costs of other states, most of which use MCOs to run their programs.
While keeping costs down and during a significant expansion in enrollment due to the Affordable Care Act (ACA), Connecticut Medicaid has not sacrificed the quality of care or members’ access to needed care. In a comparison with New Jersey, a sociodemographic match and an MCO state, researchers found that since removing MCOs, Connecticut Medicaid’s rate of early cancer detection rose 4% and survival rose 8%. New Jersey’s rate did not change over the same years.
Federal quality of care data across dozens of core measures finds that Connecticut is in the top quarter of state Medicaid programs for the majority of both child and adult quality measures. Connecticut Medicaid members are less likely to miss care due to cost and more likely to have a personal doctor than members in other states. Read more for sources

